During high school in Chicago, Dr. Clarence Shannon had a life changing opportunity - the invitation to attend a math and science summer program for minority students on the East Coast. This experience expanded his horizons on what his own potential was.
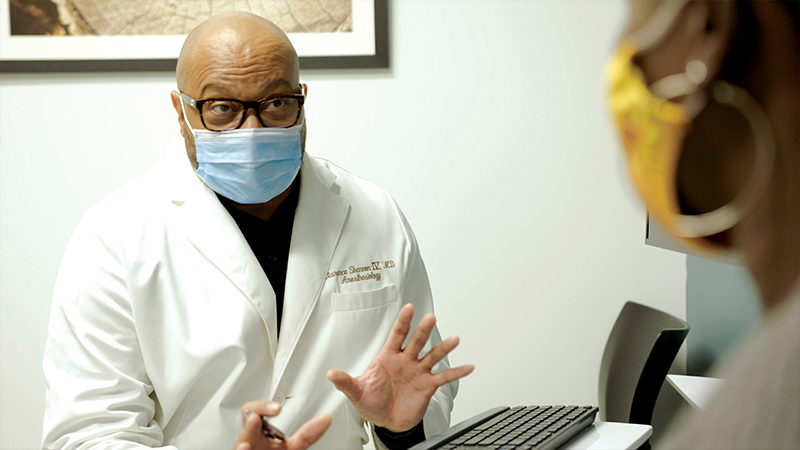
Today he is making a difference, not just for patients, but as the medical director of M Health Fairview Clinic for Comprehensive Pain Management, and by training the next generation of students and residents.
Dr. Shannon makes it clear that he owes this journey to a mentor who inspired him as a young high school student to dream bigger.
And it’s that simple humility that makes him such a bright light in the ever so dark world of pain.
Says Dr. Jakub Tolar: “We are all just a hair’s breadth away from destructive pain – pain that can bring any one of us to our knees. Dr. Shannon is exactly the kind of doctor you want in your corner.”
Dr. Shannon is, by training, an anesthesiologist. For some 17 years, he worked at the famed Walter Reed National Medical Center in Bethesda, MD.
Pain management is a natural fit for anesthesiologists who, in operating rooms every day, work with such pharmacological tools as nerve blocks.
But drugs, Dr. Shannon is quick to add, are by no means his only tool. In fact, with the rise in opioid addiction, he is focused on finding other ways to help his patients.
Among possibilities: Acupuncture, hypnosis, meditation, physical and psychological therapy, even the simple use of a foam roller for people with excruciating IT band knee problems.
“We all want the doctor to give us a pill that takes care of our problem when maybe what we really need is to get up 15 minutes early and foam roll.”

One of the biggest challenges in treating pain is that it’s subjective. One person’s three on a pain scale of one to ten can be another person’s six.
That’s why Dr. Shannon focuses more on restoring function, than reducing pain. Especially, he says, because, after years of fighting pain, we need help freeing ourselves from a negative feedback loop.
Dr. Shannon asks patients a simple, but empowering question that puts them on a measurable path to recovery: “What is something that you’d like to do, but can’t?”
Every patient is unique – requiring a different tool and maybe even a different set of tools.
But if there are similarities, one is that Dr. Shannon is often his patients’ last resort. And, by then, pain has often wrecked their careers, marriages, families, even sanity.
Dr. Shannon listens carefully to each of their stories, and then, before devising a personalized plan that often includes help from colleagues at the U, his humility comes into play.
He tells them that because of the insidious way pain works its way into not just our minds, but our lives, he can’t do this alone. He’ll need the patient to work every bit as hard in making what he calls a lifestyle change.
“There’s no quick fix. We’re going to unpeel the onion – layer by layer – and eventually get to the core as our relationship evolves.”


University of Minnesota Medical School, Medical director of the M Health Fairview Clinic for Comprehensive Pain Management
Shannon's lifelong mentor – met first in a high school summer program, and then found again in medical school – has shown him how important having someone’s support is to achieving your goals. Shannon says: “Even more than mentoring me, he nurtured me – letting me see some of the possibilities of what my life could be.”
Shannon wants to help his patients find their own possibilities by eliminating the obstacles caused by pain.

Dean of the University of Minnesota Medical School
Pain is one of the most difficult things to deal with. I treat some patients with corrosive, profound pain syndromes that prevent them from having a remotely normal life. As a physician, you want to relieve that suffering. Having an expert like Dr. Shannon, who understands the science of pain and can treat it ― not as a symptom, but as the problem itself ― is invaluable. I am glad to have him on my team both as a physician and as a leader.
Inspired
M Health Fairview Clinic for Comprehensive Pain Management